1984 Modified New York Criteria for AS
Clinical Criteria
- Low back pain ≥ 3 months, improved by exercise and not relieved by rest
- Limitation of lumbar spine in sagittal and frontal planes
- Limitation of chest expansion (relative to normal values corrected for age and sex)
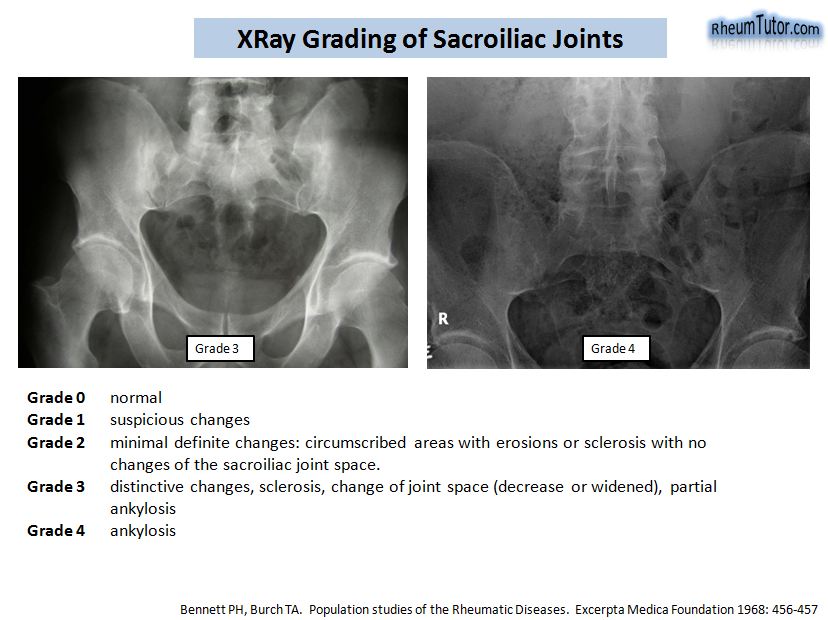
Radiological Criteria
- Bilateral grade 2-4 sacroiliitis, or;
- Unilateral 3-4 sacroiliitis
Requirements
Reference
X-Ray Grading of SI Joints
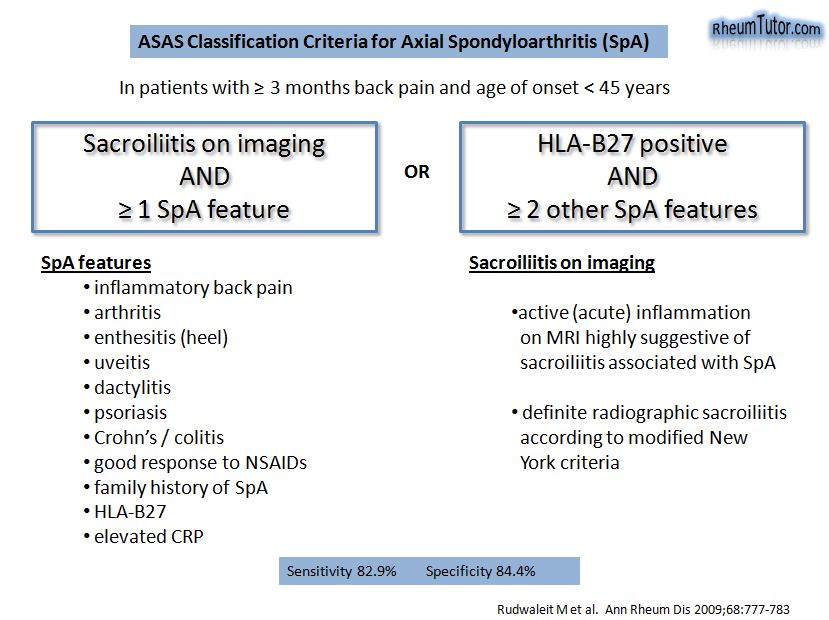
ASAS Criteria for Axial SpA
ASAS Criteria for Peripheral SpA
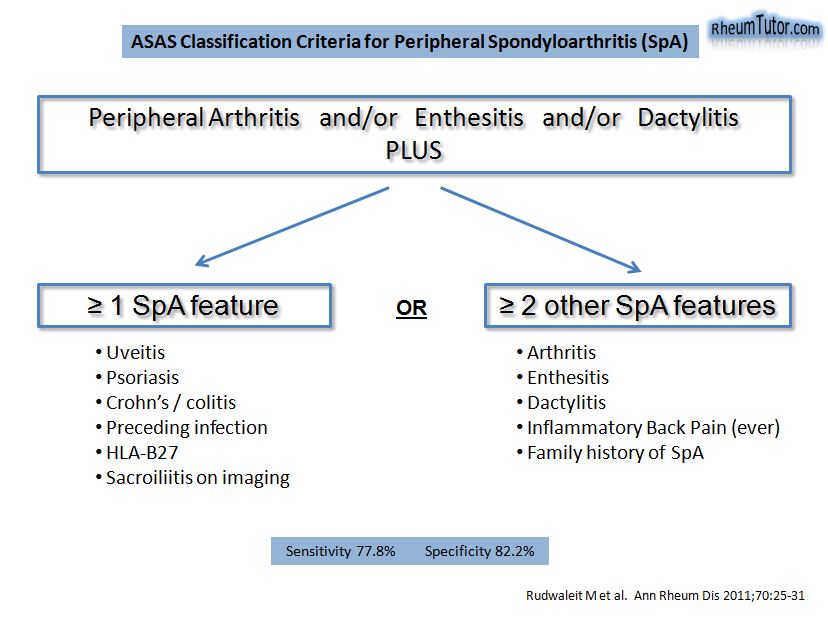
Entry Criteria
These criteria are applicable to patients with peripheral arthritis compatible with SpA (usually asymmetric and/or predominant involvement of the lower limb), and/or enthesitis and/or dactylitis.
Additional SpA Features
IBP: IBP in the past according to the rheumatologist’s judgement
Arthritis: Past or present peripheral arthritis compatible with SpA (usually asymmetric and/or predominant involvement of lower limb)
Enthesitis: Past or present spontaneous pain or tenderness at examination of an enthesis
Uveitis: Past or present uveitis anterior, confirmed by an ophthalmologist
Dactylitis: Past or present dactylitis, diagnosed by a doctor
Psoriasis: Past or present psoriasis, diagnosed by a doctor
IBD: Past or present Crohn’s disease or ulcerative colitis diagnosed by a doctor
Preceding Infection: Urethritis/cervicitis or diarrhoea within 1 month before the onset of arthritis/enthesitis/dactylitis.
Family history for SpA: Presence in first-degree (mother, father, sisters, brothers, children) or second-degree (maternal and paternal grandparents, aunts, uncles, nieces and nephews) relatives of any of the following: (1) ankylosing spondylitis, (2) psoriasis, (3) acute uveitis, (4) reactive arthritis, (5) IBD
HLA-B27: Positive testing according to standard laboratory techniques
Sacroiliitis by Imaging: Bilateral grade 2–4 or unilateral grade 3–4 sacroiliitis on plain radiographs, according to the modified New York criteria, or active sacroiliitis on MRI according to the ASAS consensus definition